By Lindsey Breunig-Rodriguez
Every year we like to provide program updates and share new curriculum. Do not worry, next month we will back to regular scheduled fruit and veggie facts.
Greetings from the McLennan County Texas A&M AgriLife Extension Service! My name is Lindsey, and I am the Extension agent for the Better Living for Texans (BLT) Program. BLT is a nutrition education program for adults and youth who are SNAP participants or SNAP eligible, and in October we kicked off our 26th year of serving Texans.
Programs are free and rooted in research. Evidence-based information empower individuals, families, and communities to make positive changes for healthier lives. Whether we meet in-person, online, virtually, or through a combination of methods, we are here to serve you. This monthly update will feature our available curriculum. You will see that BLT is for all Texans.
Curriculum Highlights:
FOCUS: NUTRITION
A Fresh Start to a Healthier You! – Target Audience: Adults
Promotes increasing fruit and vegetable intake, food safety, and food resource management.
A Fresh Start to a Healthier You! – ONLINE – Target Audience: Adults
Promotes increasing fruit and vegetable intake, food safety, and food resource management.
Conducted completely online.
Get the Facts – Target Audience: Adults
Teaches how to read Nutrition Facts Labels and identify portion sizes, sodium, fat, and added sugar found in foods.
Healthier Carbohydrates -Target Audience: Adults
Promotes a healthful eating pattern to prevent or delay diet related chronic diseases
Be Well, Live Well – Target Audience: Older Adults
Promotes nutrition and physical activity specifically targeting older adults
Color Me Healthy – Target Audience: Preschoolers and Kindergarteners
Provides fun, innovative, interactive learning opportunities on physical activity and healthy eating.
Balancing Food & Play – Target Audience: 3rd-5th graders
Promotes good nutrition and healthy weight; physical activity; limiting screen time; increase fruit and vegetable intake; drinking milk with meals and water with snacks.
Choose Healthy – Target Audience: Middle Schoolers
Teaches about MyPlate, physical activity (energy balance), making healthy food choices, and choosing healthy drinks.
FOCUS: GARDENING
Growing and Nourishing Healthy Communities – Target Audience: Adults
Teaches how to build gardens and grow fresh vegetables.
Learn, Grow, Eat and GO! – Target Audience: 3rd-5th graders
Enhances gardening skills and increased fruit and vegetable intake
FOCUS: PHYSICAL ACTIVITY
Walk Across Texas! (WAT!) – Target Audience: all ages
Promotes increased physical activity through tracking miles walked
Walk N Talk – Target Audience: all ages
Promotes increased physical activity – WAT! with added nutrition messages in a discussion format. Discussion topics are: 1. Fruits and Vegetables, 2. Rethink Your Drink! (hydration, flavored waters, sugary drinks, etc.)
If you have questions, want to plan and brainstorm, or want to hear more, please reach out to Lindsey at McLennan County’s Texas A&M AgriLife Extension office:
Phone, 254-757-5180 or email, [email protected]
Due to the continued spread of COVID-19 and the challenges it poses to communities across Texas, Texas A&M AgriLife Extension and many others continue to practice public health recommendations. Whether we are communicating online or face-to-face know that program content will always be research-backed to help individuals navigate decisions for themselves and their families. For information on resources, ideas, and programs for yourself and family visit Texas A&M AgriLife’s HUB.
USDA is an equal opportunity provider and employer. This material was funded by USDA’s Supplemental Nutrition Assistance Program — SNAP. To learn more about the Supplemental Nutrition Assistance Program (SNAP) or to apply for benefits, visit www.yourtexasbenefits.com

Lindsey Breunig-Rodriguez is an Extension Agent for the Better Living for Texans program with the Texas A&M AgriLife Extension Service. She is originally from Grapevine but now calls Waco home. A graduate from Baylor University, she loves to venture out to Cameron Park, visit the local Farmers Market, and try out the awesome eateries in Waco. If you see her and hear a loud bark, that’s her pup Lucy Ann just saying hello.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
By Jamie Willmann
In a time where much dissension exists, where the world is hurting out of a lack of love and community, and where isolation has hindered social interaction, we can find a sense of connection in the most unexpected places.
There is benefit in meeting someone who is experiencing the same trials or pain we are going through. Though we may all come from differing backgrounds, we can find unity in this COVID-19 disaster by digging a little under the surface. Underneath, we still find persons who have emotions and feelings that are directly affected by the state of the world.
Finding commonality in trials breeds possible connection. When we relate to one another, sympathy is present. It creates a sense of safety knowing that someone knows what we are experiencing. We may not feel as lonely in our trials anymore, and it creates an internal sense of validation.
People across the world are experiencing an influx of changes to their normal routines. By nature, we are adaptable to new environments and changes, but the pandemic is entirely on a new scale. It is bringing new situations that we never thought possible.
We are not designed to be isolated from others. We crave community and the presence of others. As we now adjust to something that goes against our nature, problems arise. Anxiety increases, and irritability becomes present.
In the moments when you feel COVID-19 has shattered your daily life, imagine that you are standing at the edge of potential for growth. Although you may feel anxious, depressed, or fearful, you also share in the fact that there is growth that can come out of this. You, however, have to choose that path.
The first step is acknowledging you need help and then accepting a helping hand from your neighbor.
There is a conception of mental health that needs to be stopped. Many believe they must appear as if they have it all together, which then inhibits them from receiving the help that could change the trajectory of their daily lives. We must break down these expectations to allow others in to help us.
Whether you are facing job loss, money problems, sickness, or family loss, know that you are not alone. Nowhere does it say that you have to do this on your own.
Our Crisis Counseling Program (called Texans Recovering Together) is made possible by a dedicated group of professional counselors.
— We are a team of people devoted to providing accessible, caring, and responsive services.
— We are here to listen to you, to build you up, and to provide you with what you need to press on.
— We are a network of community support that is here by your side.
By empowering our communities and taking a strength-based approach, our services provide empowerment to the community and resilience to combat the fear. We believe that we are better together, and we want to help you through these hard times.
Call us at toll-free at (866) 576-1101 to speak with a counselor, or request counseling here.
We are #TexansRecoveringTogether. We are here to help you recover.

Jamie Willmann was raised in a Christian home and was taught to serve and love others at an early age. She has a passion for making people smile and brightening people’s days. Jamie came from Wisconsin three years ago to attend Baylor, where she graduated with a degree in international studies. She now devotes her free time to self-care, exercising, relaxing in nature, and fellowship with friends.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected]for more information.
By Ferrell Foster
Five Waco civic, health, and school leaders Wednesday encouraged the people of Greater Waco to think of their neighbors and to be careful how they are involved in gatherings and celebrate the Labor Day weekend. They also stressed the importance of getting a flu shot.
With the holiday coming and football season upon us, Mayor Kyle Deaver asked residents to do these activities “smartly and safely” so the community can remain open. “Take care of yourself and take care of each other.” He made the comments during the weekly City of Waco News Conference related to the COVID-19 pandemic.
Jerry Maze, executive director for Education Service Center Region 12, noted, “What happens in the community shows up in the schools,” and that can be both good and bad. “If everyone works together and makes good decisions, we get better outcomes.”
Dr. Brian Becker, of Ascension Providence Hospital, called special attention to the holiday weekend, noting that following standard safety procedures is important for our public health and to our neighbors.
Dr. Marc Elieson, of Baylor Scott & White-HIllcrest, also spoke to the importance of wearing face masks, distancing, and proper hand hygiene. ”Be wise,” he said.
A number of questions were asked about schools and Baylor. For students, “it’s so much more about what’s happening off campus,” Mayor Deaver said. “We know this is hard; it’s trying for everyone, … but it’s the way we keep schools open and having football” and other activities.
Dr. Jackson Griggs, of the Family Health Center, praised the efforts of Baylor University to test and then isolate students exposed to COVID-19. “I’m impressed with efforts by Baylor to mitigate the risk.”
Current hospitalizations are down some, but the hospital representatives said their in-patient numbers usually lag behind case counts by about a week. And case counts have been rising in McLennan County.
The current “Effective Reproduction Rate” for McLennan County is 1.07, Mayor Deaver said. Anything above 1 means the disease is expanding, not contracting. The Rt is a measure of contagiousness or how many people one COVID-19 person infects.
In his closing remarks, Dr. Griggs highlighted the importance of bringing down the positivity rate. In recent weeks that rate has hovered just under 15% in McLennan County, which is above the state rate. More testing helps identify people with COVID-19 and also lowers the positivity rate. “Anyone with subtle symptoms needs to come in and be tested,” Dr. Griggs said. The first step is to contact your primary care physician.
The head of Family Health Center also emphasized the importance of flu vaccinations. “We need to keep flu rates down this season,” Dr. Griggs said. There’s a lot we don’t know about flu and COVID-19 infections in the same person. “Flu vaccines are imperative.”
It is especially important to promote the flu vaccines in “communities of color” because they have been particularly hard hit by COVID-19 and have “historically lower vaccination rates.”
The news conference is aired at 1:30 p.m. each Wednesday at WCCC-TV for the public to view.

Ferrell Foster is senior content specialist for care and communication for Prosper Waco. He also serves on the Act Locally Waco Board of Directors and helps the website with blog posts related to health, education, financial security, and equity.
By Paula Solano
As we to transition into the 2020-2021 school year, we can appreciate how our school and health systems work collectively to ensure the safety of students and educators. I find apples, a seasonal fruit often associated with both health and education, appropriate for this season.

Extended workdays, possible home schooling, and other responsibilities may often lead to missing a meal or making a fast-food run. The U.S. Department of Agriculture’s MyPlate provides recipes, tips, and resources to guide you in creating a healthy eating plan. Start simple, download the MyPlate App, an easy-to-use app that will help guide you and track your progress.
Apples might be the essential fruit to have in a pinch. In fact, apples can be enjoyed during breakfast, lunch, or dinner or as a perfect on-the-go snack. When selecting apples, choose those that are firm, with intact stems, and they should smell fresh.
Wash your hands as recommended by the CDC, clean contact surfaces, and thoroughly rise apples to remove any dirt before you pack, enjoy, or use while preparing a meal. Refrigerate apples in a plastic bag, away from other fruits and raw meats for up to three weeks.
Not only are apples yummy, they are saturated fat free, low in fat cholesterol, and sodium free. Apples are rich in fiber and phytochemicals (compounds produced by plants).
Enjoy these tasty apple recipes!
Apple Cinnamon Yogurt Muffins (Kid Friendly)

Serving: 24
Nutritional Information: Calories: 217, protein: 3g, fat: 10g, carbohydrates: 29g, fiber: .6g, sodium: 230mg, cholesterol: 44mg
Ingredients
1 ¾ cups sugar
3 cups all-purpose flour
3 1/2 teaspoons baking powder
1/2 teaspoons salt
1/2 teaspoon grated orange zest
1/4 teaspoon ground nutmeg
1 cup (2 sticks) butter or margarine
1 cup grated Braeburn or Golden Delicious apple
1 container (8-ounce) low fat vanilla yogurt
2 large eggs, beaten
1 teaspoon ground cinnamon
Instructions:
1. Heat oven to 350° F. Grease 24 3-inch muffin pan cups or line with paper liners. In large bowl, combine flour, 1 cup sugar, the baking powder, salt, orange zest, and nutmeg. With pastry blender or fork, cut in 3/4 cup (1 1/2 sticks) butter until mixture is crumbly.
2. In medium bowl combine apple, yogurt, and eggs; add to flour mixture, stirring until just combined. Spoon batter into prepared muffin cups and bake 20 to 25 minutes or until centers spring back when gently pressed.
3. Cool muffins in pan 5 minutes; remove from pan and cool until able to handle. Meanwhile, melt remaining 1/2 stick butter. In small bowl, combine remaining 3/4 cup sugar and the cinnamon. To serve. brush tops of muffins with butter and roll top in cinnamon-sugar mixture.
4. Enjoy!
Golden Apple Oatmeal

Servings: 1
Nutritional Information: Calories: 122, protein: 4g, fat: 2g, carbohydrates: 27g, fiber: 3g, sodium: 331mg, cholesterol: 0mg
Ingredients
1/2 cup diced Golden Delicious apple
1/3 cup apple juice
1/3 cup water
1/8 teaspoon cinnamon
1/8 teaspoon nutmeg
1/8 teaspoon salt (optional)
1/3 cup quick cooking oats (of your choosing)
Instructions:
1. In small pot, combine apple, apple juice, water, cinnamon, nutmeg, and salt (if desired); heat to boiling. Stir in oats and cook 1 minute. Cover and let stand two minutes before serving.
2. Enjoy!

Paula Solano is a Master in Public Health student at Baylor University and certified Community Health Worker who is volunteering at the Texas A&M AgriLife Extension Service. A Waco native, she is passionate about serving her community, particularly underserved and underrepresented residents.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
NEWS RELEASE
The Texas Health and Human Services Commission announced today the launch of HTW Plus, enhanced postpartum care services for eligible women enrolled in the Healthy Texas Women program. Beginning Sept. 1, about 90,000 HTW clients will automatically receive this new postpartum care coverage for up to 12 months.
While all women in HTW have access to screening, diagnosis, and medication to treat postpartum depression, women with HTW Plus coverage will also be able to receive outpatient individual, family, and group psychotherapy services, as well as peer specialist services.
HTW Plus will provide physical health, mental health, and substance use disorder services that address asthma, diabetes, hypertension, certain cardiovascular conditions, perinatal mood and anxiety disorders including postpartum depression, and substance use disorders including drug, alcohol, and tobacco use.
Approximately 90,000 postpartum women enrolled in Healthy Texas Women on average each month will be covered by HTW Plus and have access to expanded postpartum care services for up to 12 months after the date of enrollment in the Healthy Texas Women program.
HHSC will issue new HTW Plus pink cards and an updated information packet to women eligible for the new service package.
In 2019, SB 750 directed HHSC to evaluate postpartum care services provided to women enrolled in HTW after the first 60 days of the postpartum period and develop a postpartum care services package for women enrolled in HTW.
HHSC contracted with The University of Texas Health Science Center at Tyler and The University of Texas System Population Health to conduct an evaluation of services used by women in the Medicaid for Pregnant Women program in comparison to the Healthy Texas Women program. Additionally, findings from the Maternal Mortality and Morbidity Review Committee informed the HTW Plus service package.
The evaluation focused on services related to the major health conditions recognized as contributing to maternal morbidity and mortality in Texas—common cardiovascular conditions, substance use disorders, mental health conditions, and certain chronic health conditions.
Covered services include:
- Cardiovascular imaging and laboratory studies, blood pressure monitoring equipment, and antihypertensive, anticoagulant, and antiplatelet medications
- Diabetes management services including labs, additional injectable insulin options, blood glucose testing supplies, and voice-integrated glucometers for women with diabetes who are visually impaired
- Asthma medications and supplies
- Psychotherapy and peer specialist services for postpartum depression and other mental health conditions
- Screening, brief intervention, and referral to treatment (SBIRT); medication assisted treatment (MAT); and peer specialist services for the management of substance use disorders
- Tobacco cessation drugs
About Healthy Texas Women
The Healthy Texas Women program provides family planning services and other women’s health services that contribute to preconception care and better birth outcomes. The program provides a wide variety of women’s health and core family planning services, including contraception, cancer screenings and pregnancy testing. In Fiscal Year 2019, about 279,000 women on average each month were enrolled in the Healthy Texas Women program.
By Kayla Gilchrist
Oftentimes, many people confuse COVID-19 and its risks with influenza (flu), believing they are relatively the same.
“It’s not that serious; it’s just like the flu.”
“Why can’t they find a seasonal vaccine for coronavirus like they did for the flu?”
“I’ve had the flu before so I’m pretty sure I can handle COVID-19.”
Although both COVID-19 and the flu share similar characteristics, such as both being contagious respiratory illnesses, they are caused by separate viruses which bring about some vital differences.
Coronaviruses are found in both humans and animals causing mild to moderate respiratory issues. COVID-19 is caused by a completely new coronavirus called SARS-CoV-2, which causes a more severe illness. The flu is caused by influenza viruses — completely different strands of viruses than coronaviruses.

Due to some of the symptoms of the flu and COVID-19 being similar, it can be difficult to tell the difference without testing to confirm a proper diagnosis. Because COVID-19 comes from an entirely new strand of virus (SARS-CoV-2), we are learning more and more everyday.
Given the best and most updated information from the Centers for Disease Control and Prevention, below are some key differences and similarities between COVID-19 and influenza.
Similarities
1. Common symptoms shared by both COVID-19 and the flu which range from asymptomatic (no symptoms) to severe are:
- Fever or feeling feverish/chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue (tiredness)
- Sore throat
- Runny or stuffy nose
- Muscle pain or body aches
- Headache
- Some people may have vomiting and diarrhea, though this is more common in children than adults
2. For both the flu and COVID-19, one or more days can pass before an infected person starts to experience signs of illness or symptoms.
3. It’s possible to spread both viruses up to 24 hours before showing any symptoms.
4. Both can spread between people within about 6 feet or from person-to-person contact through droplets made when an infected person coughs, sneezes, or talks. These droplets can reach the mouth, nose, or be inhaled into the lungs of someone nearby an infected person. Both viruses can also spread through physical touch (e.g. shaking hands) or by people touching infected surfaces then touching their face.
5. Both COVID-19 and flu pose the highest risk to:
- Older adults
- People with certain underlying medical conditions
- Pregnant women
6. Both COVID-19 and flu can cause these complications:
- Pneumonia
- Respiratory failure
- Acute respiratory distress syndrome (i.e. fluid in lungs)
- Sepsis
- Cardiac injury (e.g. heart attacks and stroke)
- Multiple-organ failure (respiratory failure, kidney failure, shock)
- Worsening of chronic medical conditions (involving the lungs, heart, nervous system or diabetes)
- Inflammation of the heart, brain or muscle tissues
- Secondary bacterial infections (i.e. infections that occur in people who have already been infected with flu or COVID-19)
7. Anyone with a high-risk of complications and/or who have been hospitalized for COVID-19 or flu should receive proper medical care.
8. Any and all vaccinations for COVID-19 and flu must be approved or authorized for emergency use (EUA) by the FDA.
Differences
1. If you have COVID-19, it could take longer to develop symptoms than if you have the flu — up to 14 days after infection. A person with the flu usually develops signs and symptoms anywhere from one to four days after infection. Unlike the flu, with COVID-19 you may also experience a change in or loss of taste or smell as part of your symptoms.
2. If you have COVID-19, you might be contagious longer than if you have the flu. Most people with the flu are contagious up to 7 days while those with COVID-19 can remain contagious up to 10 days.
3. COVID-19 is believed to be more contagious. It’s been observed to spread quicker and more easily to a wider range of people than the flu.
4. Children are more at risk for complications from the flu than from COVID-19, however the CDC states that “both infants and children with underlying medical conditions are at increased risk for both flu and COVID-19.”
5. School-aged children pose a higher risk of a rare but severe complication of COVID-19 called Multisystem Inflammatory Syndrome in Children (MISC).
6. Those with the flu will most likely recover in less than two weeks unless they develop complications, whereas recovering from COVID-19 could take up to two weeks and even longer should complications develop.
7. The flu has FDA-approved influenza antiviral drugs to treat it and multiple vaccines produced annually for prevention. Studies, including a study on an antiviral agent called Remdesivir, which is available under Emergency Use Authorization (EUA), are still in progress on how to prevent and treat COVID-19. The National Institutes of Health (NIH) developed a regularly updated guide on treatment of COVID-19 here https://www.covid19treatmentguidelines.nih.gov
Here are resources to use for what to do if you are sick with COVID-19 or the flu and how to prevent them:
https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html
https://www.cdc.gov/flu/treatment/takingcare.htm
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/
https://www.cdc.gov/flu/prevent/index.html
Sources: https://www.cdc.gov/flu/symptoms/flu-vs-covid19.htm
https://www.ynhhs.org/patient-care/urgent-care/flu-or-coronavirus
https://www.hopkinsmedicine.org/health/conditions-and-diseases/coronavirus

Kayla Gilchrist is an adventure-seeking, fun-loving, Christ-oriented, twenty-something with an extensive background in media and a knack for writing. She received her bachelor’s in communications with a minor in theatre arts from Prairie View A&M University. When she isn’t writing or managing social media accounts, Kayla enjoys acting, directing short films, delicious food, poetry, swimming, novels, and spending time with family and friends. She happily just joined the City of Waco team and is excited to use her skills as a helpful resource during the COVID-19 pandemic.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
By Sai Sagireddy
I sit down today with a smile on my face, writing this story after ten-weeks of scrupulous research, calls, emailing, outreach, and one completed medical guide.
I must be honest. In the first few weeks, I didn’t think I could’ve taken on a project of this size. I was frequently drowning under waves of information. I didn’t know how to present what I had. I didn’t know how to continue. More often than not, I felt an urge to close my pen, shut down my laptop, and walk away. But one thing kept me going:
The thought of a disadvantaged person opening a medical guide in Waco, TX, and finding the specific healthcare service they require – free of cost.
This is the goal of the Waco Low-Income Healthcare Resources Guide.
The Start
Back in May, after committing to Baylor, I needed a medical insurance plan.
(For 15 years, I’ve lived in Trinidad & Tobago. Here, general healthcare is free – both for residents and foreigners. So health insurance wasn’t necessary).
In the US, medical costs surprised me. How can low-income families afford this? What are the resources available to them? To me, answers to these questions are so essential, especially with the COVID-19 pandemic.
From that day, I worked to comprehend the US healthcare system. I grew to understand the populations within Waco and how they receive care. Many programs cater to disadvantaged Waco residents. However, no resources are available to connect these populations to the plans, so services are potentially being under-used. I wanted to find a way to bring about awareness – a critical factor in effecting change.
Setting the Stone in Place
I brought up my thoughts with a mentor of mine: Cyrus Buckman, Stanford School of Medicine Class of 2024. He motivated me to work on improving healthcare accessibility in Waco.
A few days later, by chance, I met Ethan Lowder, WashU Class of 2022. He is the president of Heart for the Homeless, a non-profit that aims to improve the health of the homeless through primary care and knowledge. Ethan educated me further on the lifestyle and needs of disadvantaged populations. He told me about his group’s resources project and the healthcare guide for St. Louis, MO.
His expertise showed me that a healthcare resources guide detailing healthcare resources in Waco. Especially so with over twenty-nine percent of the city currently living under the federal poverty line. Upon further conversation, Ethan agreed to mentor me as I author the guide.
The Work
Over seven weeks, I’ve obtained data on healthcare institutions and programs catered for low-income Waco families. For two weeks after that, I’ve used the information gathered to “binge-write” the book.
The project also has contributions from several independent-collaborators. Juan Marinangeli translated the guide into Spanish. Ava Hunwick worked on the guide’s digital design. Sherwin Newton produced the maps. Hannah Payne connected collaborators. Matthew Gopaulchan proof-read the guide and worked on the glossary.
The Guide
The Waco Low-Income Healthcare Resources Guide contains information on over ninety medical institutions and fifteen healthcare programs that cater to low-income families and disadvantaged individuals within the Waco area. It is designed to be a vital tool for homeless individuals & needy populations directly, organizations focused on serving low-income families, and health & social service professionals.
(The guides were designed in a way for homeless populations to find a specific service within a physical copy, by themselves, easily.)
Moreover, it will help homeless shelter directors to inform individuals about healthcare options, student organizations & non-profit groups focused on service, and prehealth & health groups in the Waco area and beyond.
English:
https://drive.google.com/file/d/1SXG6rArR2JTI0Zi0tllXRJa2wexoSANJ/view?usp=sharing
Spanish:
https://drive.google.com/file/d/1qQyKN22Ry1jYQUl6KRIS7UPwwVbU3Rqi/view?usp=sharing
Funding Needs
While an online guide format is very versatile for health & social service working professionals, it will not do for homeless populations. They need physical copies.
The main focus of this project is to remove barriers to healthcare. And technology can become a barrier. These guides can be used by homeless populations directly. However, with limited computer literacy, a homeless individual within a shelter would be unable to use a digital version. They need physical copies. Moreover, in soup kitchens, physical guides can be easily used by transient members to help populations.
We are currently actively seeking funding partners to print 100 physical copies of the guide. These copies will be placed in homeless shelters, organizations, non-profit groups, and departments in Waco for low-income populations to use. They will not be removed from their home locations. They can be borrowed in-house and then returned. If interested, please contact me directly at [email protected].
My sincerest hope is that this guide will go on to help as many individuals as it possibly can.
Some things I learned
Over the past few weeks, I’ve learned a lot.
I now promote a collaborative mindset towards everything I do. This guide would not have been the same without the input & feedback from individuals: both collaborators and mentors. Collaborations allow us to combine particular strengths & skill sets to create the best outcome.
Outside of organized events & projects, I’ve also seen first-hand that creative methods and “outside-the-box” strategies can be successfully used to tackle a problem or need. All it takes is a leap of faith!
I’ve learned the importance of compassionate mentorship. Dr. Diaz-Espinoza, Associate Director of Baylor’s ALD, has been working to gather resources. He introduced me to Mr. Peacock, Assistant Director within Baylor’s External Affairs, and Dr. Beverly, SC, for Community Service. Mr. Peacock has been driving outreach efforts and has identified essential city projects the guide can be integrated with. Without this care and time, our distribution efforts may have been much more challenging.
Final thoughts
Reading back over what I have written makes me think: wow, it has been quite a journey.
Going in, I was lost. I didn’t know where to begin. What to do. Now, I have authored the Waco Low Income Healthcare Resources Guide, a medical services book that contains comprehensive information about the healthcare services available to the needy within Waco. It acts as a bridge that connects these populations to medical services via independent community-based organizations.
Throughout this journey, I’ve found a community equally passionate about service. I’ve gained mentors nationwide who share my goals. I’ve developed a malleable skillset that I can use within my academics and projects. I’m forever grateful!
This guide’s digital edition will soon be available through several online local and regional databases for use. However, we are still actively seeking funding for physical copies.
If you have any questions whatsoever about the project, if you want to get involved in this effort or future project, or if you are a potential financial collaborator, please reach out directly to [email protected].

Sai Sagireddy is an incoming freshman at Baylor University. He is part of Baylor’s University Scholars Cohort Class of 2024 with concentrations in biology/biochemistry, Spanish, and medical humanities (pre-med). He is passionate about research, global health, healthcare management, health equity & health accessibility. In his free time, he enjoys the company of others, settling down a good book, exercising, hiking, traveling, and exploring the outdoors.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
By Lindsey Breunig-Rodriguez
Recently I have been thinking about the “Wild West” — a time when there was a lot of discovery and a lot of unknown. I must say, it somewhat feels like we are in a modern-day Wild West. I can only imagine how difficult it was to stay hydrated. Someone probably shared a water canteen and planned travels according to where the next water source would be.

Today we do the same when we camp, go hiking or walking, or are outside for an extended time. To avoid dehydration, we must actively think about drinking more water, and even more so in these hot summer months.
Thankfully, we do not have to solely rely on water; fruits and vegetables also provide us with water. This month we are highlighting a vegetable which consist of 95% water, making it a great source for extra hydration and is even named for its season. Introducing summer squash!
Nutrition:
Per USDA dietary guidelines it is recommended we consume 3 Cups of vegetables daily. Vegetables may be fresh, canned, frozen, or dried, and may be whole, cut-up, or pureed. It all counts!
Summer squash is a great source of vitamin C, which keeps our immune system strong and helps our bodies heal quickly. Additionally, summer squash is fat free, saturated-fat free, sodium free, cholesterol free, and low in calories (around 20 calories in 1 cup). It is not recommended to peel summer squash because most all the vitamins and minerals are found in the skin.
Shopping, Storage, and Preparation:
There are two types of squash: summer and winter. Today we are focusing on summer squash. There are many varieties of squash, some names you will see are: patty pan, yellow crookneck, yellow straightneck, chayotes, and zucchini. For all squash varieties, choose firm, glossy, small to medium-sized squash. Avoid squash that is soft, moldy, or sunken in spots. Though usable, larger squash tend to be less flavorful and tougher.
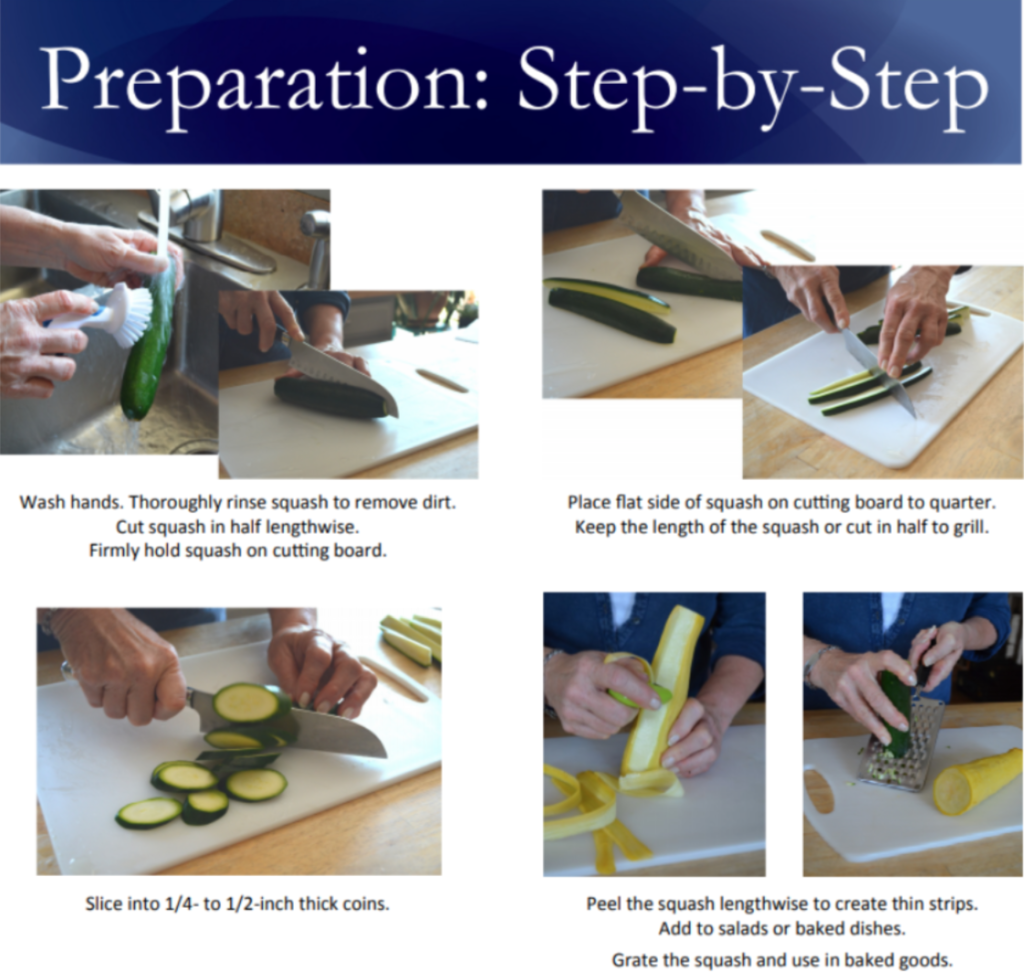
Right before using, wash squash by rubbing the skin under cool running water. Refrigerate summer squash for up to one week or freeze and use within three months. If freezing, cut it into pieces and blanch (placing vegetables in boiling water for a short time and then placing in freezing water.). For more instructions, read here.
Enjoy:
Due to its mild flavor summer squash can be prepared multiple ways. It is important, however, to remember that seasonings or other ingredients added to squash will change the nutritional value. Below are some ways to enjoy it:
Roast — Cut squash in slices and drizzle with olive oil and low‐sodium seasoning before placing on a baking sheet. Cook 10-15 minutes or until tender.
Grate — Add raw, grated squash to green salads, muffins, or cookies. Use a vegetable peeler to make ribbons in place of pasta noodles.
Grill — Pair squash with tomatoes, onions, mushrooms, peppers, or fruit.
Raw — Enjoy in salads or dipped in hummus or a low-fat dip.
Sauté — Heat pan to high, add oil to coat the pan and add sliced squash. Sauté until lightly brown, about 3‐5 minutes, or tender. Use as side dish or add to dishes like stir fry or pasta.
Check out these other tasty recipes too: Italian Spinach and Zucchini Meatballs or Baked Zucchini Sticks
See below different ways to cut and prepare zucchini – thank you to Montana State University Extension for the graphic:
Texas A&M AgriLife Extension
Due to the continued spread of COVID-19 and the challenges it poses to communities across Texas, Texas A&M AgriLife Extension and many others continue to practice public health recommendations. Whether we are communicating online or face-to-face know that program content will always be research-backed to help individuals navigate decisions for themselves and their families. For information on resources, ideas, and programs for yourself and family visit Texas A&M AgriLife’s HUB.
USDA is an equal opportunity provider and employer. This material was funded by USDA’s Supplemental Nutrition Assistance Program — SNAP. To learn more about the Supplemental Nutrition Assistance Program (SNAP) or to apply for benefits, visit www.yourtexasbenefits.com

Lindsey Breunig-Rodriguez is an Extension Agent for the Better Living for Texans program with the Texas A&M AgriLife Extension Service. She is originally from Grapevine but now calls Waco home. A graduate from Baylor University, she loves to venture out to Cameron Park, visit the local Farmers Market, and try out the awesome eateries in Waco. If you see her and hear a loud bark, that’s her pup Lucy Ann just saying hello.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
(From Waco’s COVID-19 Community Newsletter)
As the Central Texas community participates in demonstrations and protests against the killing of George Floyd and continued racial injustice and inequity, community leaders encourage health and safety precautions for group gatherings. Dr. Iliana Neumann of Family Health Center shares a few health tips for community members participating in protests and demonstrations.
We encourage organizers to provide masks and hand sanitizer to the extent they can and to model the use of such as well as practice physical distancing as much as possible.
- Assembling does increase your risk of contracting COVID-19, but there are things you can do to lessen this risk.
- Gather outside rather than inside.
- Wear a cloth face covering.
- Physically distance as much as possible.
- Do not share signs or markers with anyone who is not a member of your household.
- Take hand sanitizer and gloves with you. Use hand sanitizer often.
- If distributing materials, encourage folks to take a picture of the materials with their phone instead of handing off paper or other items.
- Bring water and drink it often.
- Wear sunscreen.
- Reduce respiratory droplets by focusing on signs/posters and making noise with music, drums, etc. rather than loud talking.
- Carry identification and a list of emergency contacts.
- Go with a buddy and stay closer to them rather than new contacts.

Dr. Iliana Neumann is a family medicine specialist. She graduated with honors from East Carolina University School Of Medicine in 2009. She is a faculty physician with Waco’s Family Health Center.
Press Release – The Waco-McLennan County Public Health District, Ascension Providence, Baylor Scott & White, and the Family Health Center have formed the McLennan County Leadership Response Team to work and plan together on a local response to reports on the COVID-19 outbreak in the country. Meeting weekly as a group, we are actively monitoring patients for risk factors and working to ensure our local health care system is prepared to respond to the situation as it unfolds.
There has been a lot of information in the news about COVID-19. If you are healthy, your risk is relatively low and recovery is high. The good news is that the same steps you can take to stay healthy during the flu season will protect you from many viruses, including the flu and COVID-19. The Response Team has prepared a list of important facts to help people understand the current situation. This is a rapidly evolving situation and the Response Team will provide updated information as it becomes available.
Risk
- There are NO diagnosed COVID-19 cases in McLennan County.
- At this time, if you have not traveled to an effected area or have not had contact with someone with COVID-19, your risk is low. Any respiratory symptoms you might have are more likely to be flu or another respiratory illness.
- Most cases of COVID-19 are not severe. People with a greater risk of developing serious symptoms are Older adults; People with chronic conditions; and People with compromised immune systems.
Symptoms
- Fever
- Cough
- Difficulty Breathing
Facemasks
- Facemasks are NOT recommended for people who are well. The use of facemasks are crucial for health care workers and other people who are taking care of someone infected with COVID-19 in close settings (at home or in a health care facility).
- You should only wear a facemask if a healthcare professional recommends it.
Protection
There is currently no vaccine to prevent COVID-19 infection. The best way to prevent infection is to avoid being exposed to this virus. The Waco-McLennan County Public Health District (PHD) encourages everyone to follow preventive actions to help prevent the spread of respiratory viruses, including:
- Wash your hands often with soap and water for at least 20 seconds. If soap and water are not available, use an alcohol-based hand sanitizer with 60%-95% alcohol.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Avoid close contact with people who are sick.
- Stay home when you are sick.
- Cover your cough or sneeze with a tissue, then throw the tissue in a lined trash can.
- Clean and disinfect frequently touched objects and surfaces with regular household products.
Isolation and Quarantine
- Your healthcare provider or the Public Health District may ask you to stay at home in order to slow the spread of the virus. Please follow the instructions given to you.
Questions
People with questions can call the Public Health Information line at 254-750-1890 which is available Monday through Friday from 8am – 5pm.
Information
This is an rapidly evolving situation and Public Health District will provide updated information as it becomes available. The most trustworthy sources for information are:
- Waco-McLennan County Public Health District;
- Texas Department of State Health Services;
- Centers for Disease Control and Prevention; and
- World Health Organization.