By Glenn Robinson
One of the hallmarks of the information age economy is consumerism – in this instance, defined as businesses making their goods and services more convenient, affordable, or otherwise desirable to customers.
For years, virtually every segment of our economy has embraced this trend… except healthcare. At least until recently. Increasingly, healthcare consumers are expecting that their experience with healthcare providers mirror the experience they have with some of the world’s top brands.
This rise in healthcare consumerism will continue according to a recent brief by Rice University’s Baker Institute for Public Policy. Not only have consumer expectations and experiences with other industries helped drive this trend, but so has the increasing popularity of high deductible health plans and incentives offered to those covered to make cost-effective choices.
In other words, as the financial burden of healthcare decision-making shifts to patients, patients are more apt to become more conscientious and expect more out of those rendering healthcare services.
This trend towards healthcare consumerism has already led to many noticeable changes in industry practices. The growing number of convenient walk-in clinics and the introduction of telemedicine are manifestations, as is the increasing focus healthcare providers put on patient experience surveys and online reviews. An entire cottage industry has grown up around healthcare design and construction to make the care environment more warm, welcoming, and comfortable.
However, one big obstacle still remains to true healthcare consumerism – pricing transparency.
It’s a complex issue, but one many organizations are working to solve.
You know having a health insurance policy is important, but equally as important is understanding what is in the policy so you can plan accordingly. Unfortunately, much of the language used in health insurance plans isn’t part of the everyday vernacular. With that in mind, here are some common terms and what they mean.
A premium is the amount of money you or your employer pays monthly or annually for your health insurance.
The deductible is how much you must pay out of pocket before your insurance starts to pay. Keep in mind, though, many preventive health services don’t require you to pay a deductible.
Co-insurance is how much you must pay out of pocket even after meeting your deductible. For instance, 80/20 co-insurance means you’re still responsible for paying 20 percent of charges.
This is different from a co-pay, which is a flat fee – for example 20 dollars – you might have to pay for a doctor’s visit.
Maximum out-of-pocket expenses are the most amount of money you will be required to pay per year for deductibles and co-insurance.
The term covered expenses refers to what medical services or prescriptions are or aren’t paid for by a plan.
Beyond these terms, if you don’t understand something about your plan, how it works, and what it covers, you can call the toll-free number on the back of your health insurance card. Most reputable insurance companies have staff trained to explain the ins and outs of every policy.
Most Americans appear to believe: your health is your wealth. While wealth sometimes can create its own problems, health inevitably is a source of happiness… and the value of health increases with age, usually surpassing the importance of wealth.
If you had a choice, would you spend your time striving for health or wealth? A majority of Americans pick health, according to a survey by TD Bank. The company surveyed over 1,000 U.S. consumers who made a 2018 New Year’s resolution.
The top goal of respondents was to eat better, with 54 percent citing it as their priority. The top financial goal was to save more and spend less, with 39 percent selecting it as a priority. Millennials – young adults between ages 22 and 37 – said eating healthy and getting in shape or staying fit is more important than saving more and spending less money.
Health and wealth are not mutually exclusive. About 41 percent of those who indicated they were satisfied with their financial health are more likely to be satisfied with their physical health, emotional health, and family well-being.
People with good health are more likely to have the energy and stamina to excel in the workplace, and they are less likely to spend time and effort dealing with the debilitating effect of chronic health conditions and disabilities.
Although most respondents said they are less confident they will achieve their goals to get in shape, they are more likely to seek advice for financial issues. Health typically is something that you earn if you are persistent and disciplined – it cannot be bought.
This report, and other episodes, are available at KWBU.org.
 Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30 years of experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30 years of experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
By Glenn Robinson
When it comes to technology that makes our lives better, the trend has been smaller, faster, and better. When it comes to next generation medical procedures being rolled out nationwide, that trend has largely been mirrored.
Procedures that once took hours, now may take only minutes. Procedures that once involved long, unsightly incisions, are now being conducted with tiny tools that may only require an incision the size of a razor nick.
Perhaps nowhere have these advancements been more pronounced than in heart care and orthopedic medicine. Take, for example, procedures to repair or replace damaged valves in the heart. Ten years ago, these procedures often involved major invasive surgery, a week or more in the hospital, and months of recovery.
Today, many of the nation’s leading heart programs – including right here in Texas – offer solutions for certain valve problems that are so minimally invasive, qualified patients can leave the hospital in as little as one day and be fully recovered within a matter of weeks.
Similarly, major orthopedic procedures, particularly in the field of joint replacement, have come a long way since the turn of the century. Advances in pre-procedure imaging, artificial devices, and operational technique have led to artificial hips and knees that feel as good as the original with a fraction of the recovery time.
These and many other innovative procedures are creating better outcomes and giving more patients the opportunity to improve their quality of life. But how do scientific studies performed in labs turn into these actual medical treatments?
Translational medicine transforms basic scientific discoveries into innovative therapies for patients. This kind of research, often referred to as “bench to bedside,” seeks to implement evidence-based medicine safely, effectively, and as quickly as possible.
One of the most challenging aspects of translational medicine is gaining widespread adoption of new, evidence-based medical practices. It takes the complete commitment of an organization’s top management to recognize and reinforce the importance of this kind of research and its comprehensive, consistent application.
Many leading health care organizations are represented through research institutes, which facilitate translational medicine. These institutions focus on basic science, clinical trials, and healthcare quality-of-care research. They seek to understand the basis of a disease, identify potential treatments or preventive therapies, and enroll patients in research trials.
The institutes’ objectives are not only to make new scientific discoveries, but to implement research successes into community-based healthcare practices and then promote proven prevention and treatment strategies throughout the entire organization and greater healthcare community.
These institutes have been responsible for creating several novel therapies right here in Texas and have attracted millions in grants from U.S. and international government agencies to support important research efforts – turning laboratory research into new standards of care for the entire industry.
Another new trend in the world of research is the use of artificial intelligence, or A-I. A-I can solve complex problems that exceed human capabilities. Through its ability to access vast troves of data, A-I algorithms can both exceed the knowledge of experts, and augment the abilities of non-experts.
A-I already is disrupting transportation, marketing, and financial services, among other sectors of the economy. In healthcare, this technology is gaining momentum and has the potential to significantly alter the industry not only by developing new treatment options, but also by streamlining back office operations.
As care providers look to better engage patients and improve efficiency, many are turning to artificial intelligence to help them succeed. A-I powered medical assistants can book appointments, remind patients to take their pills, monitor a patient’s health status, and perform other time-intensive tasks.
A survey of health consumers found 55 percent are willing to engage with A-I and robots for healthcare needs. At a recent South by Southwest conference, Mark Rolston of Argo Design said artificial intelligence and virtual reality will be important parts of healthcare’s future.
Likewise, Oscar Salazar, of the app Pager, said that A-I gives nurses “superpowers.” He predicts that A-I increasingly will take over decision-making for healthcare triage and diagnosis, dramatically changing the roles of healthcare professionals.
Don’t expect your doctor to be going away anytime soon though. Like many technologies, A-I works best when paired with smart, capable people.
This report, and other episodes, are available at KWBU.org.
 Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30-years of experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30-years of experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
By Glenn Robinson
Pop quiz. Are the Baby Boomers – people born between 1946 and 1964 and now entering their retirement years – more or less healthy than previous generations? The assumption has long been that they are.
Not only has Americans’ life expectancy increased in recent decades, we also are healthier later in life. Since the early 1990s, the average 65-year-old has gained an extra nine months of life expectancy, but gained a full year of disability-free life on average. Research bears out that the change in disability rates has been substantial. In the early 1980s, one in four elderly people had difficulty living independently. Today, there are fewer than one in five.
In addition, despite a major increase in the number of elderly in our country, the nursing home population today is virtually the same as it was two decades ago – yet another testament that the health of the population is improving, even as more people live to older ages.
David Cutler, an economics professor at Harvard University who researches disability, has reached the conclusion that people in general are in much better health right up until the last year or two of life. This is in stark contrast, he says, to previous generations in which people spent their final six or seven years of life being very sick and in and out of the hospital.
Boomers were the first generation to have greater access to healthcare and services such as regular immunizations, preventive care, and widespread use of antibiotics. They also grew up in a generally prosperous economy, and many benefitted from greater educational and employment opportunities compared with earlier generations.
All these factors positively correlate to being healthier. Research comparing Baby Boomers with people from two decades ago in the same age bracket also shows that Boomers are healthier in some important ways, including being less likely to have emphysema or suffer heart attacks.
Two critical factors have played a vital role in dropping mortality rates from heart disease. First is the slow and steady decline in smoking rates over the past half-century, which is a critical risk factor for heart disease. According to the Centers for Disease Control, in 1965 more than 42 percent of adults smoked. By 1993, that number tumbled to 25 percent, and, as of 2015, only about 15 percent of adults were smokers.
While the decline in smoking is a big win for public health, the advancements in detection and treatment of heart disease is the major success story in medicine over the past two decades. From blockbuster new cholesterol and blood pressure medications being given more often to the right patients at the right time, to groundbreaking new imaging heart technologies and minimally invasive procedures straight out of a science-fiction novel, the medical advances to manage all facets of heart disease are perhaps unparalleled in medicine.
This may all paint a bright picture, but many of these positives are offset by the negative impact of weight-related health problems. The proportion of Baby Boomers with diabetes, high blood pressure, and obesity is increasing, so the answer to whether or not Baby Boomers overall are healthier than previous generations is somewhat mixed.
One solution to this lies in the concept of preventative care.
Nine out of 10 pet owners know when their dog or cat is due for their shots. Eight in 10 mothers know their child’s sports schedule by heart, and 80 percent of men know how often they should have their oil changed. Yet only 50 percent of family health care decision makers know their blood pressure, and only 20 percent know their own key biometric numbers such as cholesterol and body mass index.
While Americans are great at preventive care for their pets and cars, it appears that is not the case when it comes to their own health. This issue puts pressure on the entire health care system because the old adage, “an ounce of prevention is worth a pound of cure,” holds true to this day.
Preventive care such as regular check-ups and practicing a healthy lifestyle help individuals avoid or delay disease. It also can help people catch a health problem early on, when it is most treatable. The Affordable Care Act requires new private health insurance plans to fully cover the costs of 45 recommended preventive services. This means patients pay no deductibles or copayments, or otherwise share costs of these services.
Unfortunately, a Kaiser Family Foundation poll found that less than half of Americans were aware of the change, meaning many people may be avoiding preventive care out of cost concerns. To make sure you’re not one of them, take advantage of these preventive services when you go in for your annual check-up.
For all the challenges surrounding health care in America, this is one of our healthcare system’s good-news stories.
This report, and other episodes, are available at KWBU.org.
 Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30 years of experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30 years of experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
By Glenn Robinson
Each year, thousands of Texas patients must rely on charity care to receive the medical services they need. Hospital charity care means no payment is expected for the services the hospital provides, which means that patients who qualify for such care typically receive no hospital bill and are not subject to collection efforts.
While Texas may lag far behind other states when it comes to number of residents who have health insurance coverage, it was the first state to establish a required level of community benefit for non-profit hospitals in exchange for state tax exemption.
This community benefit requirement means that Texas not-for-profit hospitals must spend four percent of expenses on charity care, and a total of five percent overall on charitable activities.
While exact criteria to receive hospital charity care may vary, generally patients who receive care at a non-profit hospital may apply for complete or discounted charity care if they are either financially indigent – meaning they are uninsured or underinsured with an income at or below 200 percent of the federal poverty level; or are medically indigent – meaning their medical or hospital bills exceed a certain percentage of their annual income after payment by insurers, leaving them unable to pay the remaining bill.
A hospital’s total uncompensated care is the sum of its charity care provided and uncollectable patient debt. Since 2000, U.S. hospitals have provided more than $538 billion in uncompensated care.
Funding for Medicaid and the Children’s Health Insurance Program recently have been the topic of a lot of hot political talk in Congress, so let’s take a closer look at these two government-administered health insurance programs.
Medicaid covers about one in five Americans. It reaches many low-income children, adults, seniors, and people with disabilities.
In Texas, children, the disabled, and seniors represent 90 percent of those covered by Medicaid. The remaining 10 percent are working-age adults – three-quarters of whom are employed, but do not earn enough to afford health insurance or do not work for an employer offering insurance.
Medicaid is the nation’s major source of long-term care financing, which is particularly important in supporting seniors and helping relieve the care burden that often falls on families. It also provides benefits for people with disabilities who are unable to find or afford other coverage.
The Children’s Health Insurance Program, or CHIP, is low-cost health coverage for children of families who earn too much money to qualify for Medicaid.
Medicaid, together with CHIP, has resulted in improved access to care for children and helped bring the uninsured rate for children to record lows. Children with Medicaid or CHIP have greater access to care than uninsured children and comparable access to children with employer-sponsored insurance.
But enrollment in Medicaid and CHIP have positive impacts on children and families beyond improving access to health care services. These programs may provide financial protection for families who have very little otherwise.
When we talk about a changing approach to healthcare in this country, many people’s minds immediately go to what is going on in Washington regarding healthcare policy – or perhaps some of the latest and greatest treatment technologies.
These are indeed important, impactful facets of the changing healthcare landscape, but perhaps even more impactful is the shifting mindset of many hospitals and healthcare organizations who are now focusing on overall community wellbeing.
Central to these efforts are innovative and effective community partnerships. Through community partnerships, hospitals and health systems seek out new and nontraditional partners to improve both health and overall quality of life in the communities they serve – regardless of the ethnic, racial, socioeconomic or physical circumstances that make up a community.
These non-traditional partners for hospitals may include police and fire departments, food banks and grocery stores, community recreation centers, churches, and local non-profits addressing issues such as housing and education.
The esteemed Robert Wood Johnson Foundation believes hospital-community partnerships are indispensable when it comes to building what it calls a “Culture of Health.” While often viewed as non-traditional, these partnerships make good sense because good health is dependent on far more than the medical care available to a community. A safe environment and dependable access to healthy foods are essential to the cause, as are a range of other factors.
These partnerships have the potential to reshape communities and change lives. And in the end, isn’t changing lives for the better what great healthcare is all about?
This report, and other episodes, are available at KWBU.org.
 Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30 years experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30 years experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
(During these last few weeks of December we will be reprising the Top 10 Most Opened Blog Posts for 2018 from the Act Locally Waco blog. I couldn’t possibly pick my favorites – so I used the simple (cop out?) approach of pulling up the 10 blog posts that got the most “opens” according to our Google Analytics. It is an intriguing collection that gives at least a little insight into the interests and concerns of Act Locally Waco readers. I hope this “Top 10” idea inspires you to go back and re-read your personal favorites. There have been so many terrific ones… If you would like to see the Top 10 according to Google Analytics, here’s the link: Top 10 Most Opened Blog Posts of 2018. Merry Christmas! — ABT)
By Christy Perkins
The Community Health Worker Initiative is an innovative program designed to bridge the gap between the community and available resources. The program methodically targets 4 zip codes in Waco that could benefit from these resources: 76704, 76705,76706, and 76707. As Community Health Workers (CHW) we are trained to respond to cultural diversity with understanding and acceptance to help clients overcome barriers to using the available health resources. Our role is to connect clients to resources and help them navigate the healthcare system. By doing so, we help individuals reach a state of self-sufficiency to create a healthy and thriving community. We aim to build trusting relationships with our clients, to increase basic and critical health education that will develop confidence in those facing adversity, and to decrease unnecessary emergency (E.R) visits.
In 2016, I began purposefully researching and embedding myself into organizations and projects that are geared toward advocacy and health. I became passionate about client advocacy after personal life experiences left me in the dark about such services. When my oldest son fell ill as an infant, I didn’t know that patient advocates were available to help me manage this uncertain and scary time in my life. No one stepped in to advocate on our behalf by making me aware of available services that could support my son. That is when I became prayerful and intentional in regard to advocacy and awareness. I grew interested in holistic methods of health during that time and now find myself on the path to become more educated in this area. I saw this opportunity with the Waco-McLennan County Public Health District as a foot in the door to professionally connect to, advocate for, and educate individuals who have been left in the dark like I once was. I aspire to be a voice for those who feel their voice has been silenced.
In preparing to become a CHW, my coworkers and I underwent 160-hours of training over the course of 4 months to become certified by the Texas Department of Human Services (TDHS). The training covered 8 core competencies: communication, interpersonal, service coordination, capacity building, advocacy, teaching, organizational, and knowledge base skills. During training, we began attending coalition meetings, community meetings that were open to the public, toured facilities of community organizations, and had several guest speakers who assist the community explain their services. Additionally, I’m an active participant in Leadership Plenty, Round 7, which builds skills in community leadership, managing conflict, diversity, and taking action. The CHW training together with the leadership training are important tools when working with clients and partners.
Now that my fellow CHW’s and I have completed our training, we are preparing our first project! We will be hosting launch parties in the 4 zip codes that are the focus of this program. This will be an opportunity for the community to become familiar with the CHW’s assigned to their neighborhoods as well as enjoy the festivities that we and our community partners will have available to the families. Check out our new Facebook page — McLennan County Community Health Worker Initiative — for updates on these events!
I am truly looking forward to helping my CHW team in piloting this program. I feel the beauty of this program is that we are able to meet our clients where they are in their current life situation and create an action plan that is attainable within our capacity. My hope is to assist them with self-reliance when developing goals they desire to achieve and that will be beneficial to their well-being. In turn, creating a partnership with those clients to assure them I am dedicated to their personal successes. I will strive to access integrative resources on their behalf while preparing them to confidently do so independently. My personal goal is to specialize in nutrition and help guide others in holistic lifestyle choices to improve their quality of life.
I look forward to continuing to build relationships with community partners to tackle the problems of our community by collecting information at the grassroots level that will support and develop this program. We will be working closely with the healthcare system in Waco to assure that this program is effectively aiding the community.
I’m looking forward to working with my fellow CHW’s in beginning walking groups within the communities we are serving. This is an example of the kinds of efforts that will help us connect with fellow residents and encourage healthy lifestyle routines. This is an exciting time for us as we embark on a mission that will shape a program that has been conjured up through discussion, data development, and planning for years. What an honor it is to be entrusted as the charter group to thrust this project into a flourishing program!
 Christy Perkins is a certified Community Health Worker for zip code 76707. She currently serving on the Garden Committee at Brook Avenue Elementary. She is looking forward to becoming a graduate of the prestigious leadership training with the Leadership Plenty Institute in March of 2018 and serving on the YMCA, Young Junior Professionals Board. When she isn’t involved in community work, she is a Mother of 3 handsome boys. They keep her life busy and entertaining. She has a passion for writing, reading, and fellowship. She is originally from Amarillo, Tx but has grown to love Waco, Tx and is looking forward to building a future here. You can reach her at [email protected] or on Facebook at McLennan County Community Health Worker.
Christy Perkins is a certified Community Health Worker for zip code 76707. She currently serving on the Garden Committee at Brook Avenue Elementary. She is looking forward to becoming a graduate of the prestigious leadership training with the Leadership Plenty Institute in March of 2018 and serving on the YMCA, Young Junior Professionals Board. When she isn’t involved in community work, she is a Mother of 3 handsome boys. They keep her life busy and entertaining. She has a passion for writing, reading, and fellowship. She is originally from Amarillo, Tx but has grown to love Waco, Tx and is looking forward to building a future here. You can reach her at [email protected] or on Facebook at McLennan County Community Health Worker.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
By Glenn Robinson
Health care is among the most heavily regulated industries in America – virtually every aspect of the health care system is subject to government oversight.
There are regulatory mechanisms to supervise the doctors and professionals who render care; the institutions in which care is provided, such as hospitals and clinics; the medications and medical devices that are the tools of care; and the insurance coverage that finances it all. These regulations are developed and implemented by all levels of government — federal, state and local — as well as private organizations.
Everyone in health care agrees that regulations and standards are necessary to ensure compliance and to provide safe health care to every patient. Policy debates, for the most part, typically focus not on whether oversight should exist, but rather on how it should be structured. Impartial, external oversight is considered necessary to protect the public interest – even by those who are especially suspicious of government bureaucracy.
American health care has flourished over the past 100 years. Rather than hindering its progress, the complex system of government regulation actually may have served to support and nurture it.
Consider, for example, the public confidence engendered in the competence of physicians through licensure requirements and in the safety and effectiveness of prescription drugs through the Food and Drug Administration’s approval process.
Another form of regulation is known as HIPAA. At some point while filling out a bevy of forms at the doctor’s office, you may have run across this term.
The Health Insurance Portability and Accountability Act, or HIPAA, was passed by Congress in 1996 and was intended to improve health care efficiency by standardizing electronic data exchange and protect the privacy of patient records.
Since 2010, as part of national health care reform, there has been increased urgency in transitioning to digital versions of patients’ paper charts called electronic health records, or EHRs.
EHRs can contain a patient’s medical history, diagnoses, medications, treatment plans, immunization dates, test results and more. But they’re not just a replacement for paper charts.
Part of what makes EHRs so powerful is that they also allow doctors and other care providers to access evidence-based tools that can be used to make decisions about a patient’s care in real time.
Another key advantage of EHRs is convenience. Health information can be created and securely managed digitally by authorized providers and shared with other providers at other locations.
This helps cut down on the number of forms patients must fill out and can eliminate the need for duplicate testing, as well as promote legible, complete medical documentation for streamlined coding and billing.
With all this information available to be shared with the touch of a button, precautions must be taken to ensure the privacy of the patient. As EHRs continue to evolve, so must our regulation of them.
The HIPAA law’s privacy standards strive to give patients rights over their health information, and set boundaries on who can receive a patient’s personal health information. Those who must follow the law include healthcare providers such as hospitals, doctors and nurses, pharmacies, insurance companies, and government programs such as Medicare and Medicaid.
The law limits the use of patient information by health care providers to specific purposes. Patient information can only be shared if it is necessary to coordinate treatment, pay providers for patient care, protect public health, assist police in criminal investigations, or assist family, relatives or friends responsible for care or paying medical bills – unless the patient objects.
HIPAA also requires healthcare providers to inform patients how they may use and share their health information, and grants certain rights to patients regarding their health information, such as receiving copies of their health records upon request and being informed if their health information is being used or shared.
If you are ever concerned that your personal health information is being improperly used or shared, you have the right to file a complaint either with the federal government or your healthcare provider.
So while regulation may be seen merely as red tape in some industries; in health care, it provides a critical public protection.
This report, and other episodes, are available at KWBU.org.
 Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30 years of experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
Glenn Robinson is the President of Baylor Scott & White Medical Center – Hillcrest. He has over 30 years of experience in hospital and health care management, and currently serves on several Boards associated with the Texas Hospital Association and the American Hospital Association. In addition, Glenn is Past-Chair and an active member of the Greater Waco Chamber of Commerce, and serves on the Prosper Waco Board.
by CeRon Ford
Cheeseburgers and French fries have you down in the gutter? Tired of paying for expensive salads at drive-thru restaurants? Do you want to work out but not sure where to go? No need to waste any more time searching for the most affordable salad or settling for just any gym– we have everything mapped out just for you!
 Ever heard of the Live Well Waco (LWW) Asset Map? No? Well, you may want to pay close attention to this. Live Well Waco is a coalition dedicated to improving the health of people living, working and playing in McLennan County. The Live Well Waco Coalition began more than 5 years ago as a collaborative effort between community businesses, organizations, and individuals who are dedicated to the health of McLennan County residents. LWW focuses on improving area health disparities by hosting events such as community cooking demonstrations, physical activity programs, and more. The Live Well Waco Leadership team created the asset map to promote a better understanding of diversity within the community while helping community members locate fresh produce and healthy foods, exercise facilities, healthcare facilities, and other local resources.
Ever heard of the Live Well Waco (LWW) Asset Map? No? Well, you may want to pay close attention to this. Live Well Waco is a coalition dedicated to improving the health of people living, working and playing in McLennan County. The Live Well Waco Coalition began more than 5 years ago as a collaborative effort between community businesses, organizations, and individuals who are dedicated to the health of McLennan County residents. LWW focuses on improving area health disparities by hosting events such as community cooking demonstrations, physical activity programs, and more. The Live Well Waco Leadership team created the asset map to promote a better understanding of diversity within the community while helping community members locate fresh produce and healthy foods, exercise facilities, healthcare facilities, and other local resources.
The asset map includes a list of locations that provide access to healthy living opportunities all within the City of Waco. With the LWW Asset Map, we want to help protect and conserve the local traditions, customs, and resources that are prevalent in Waco, Texas.
Maps can often be tricky, but the best way to learn is just to dive in!
Here’s the link: www.batchgeo.com/map/livewellwaco
And here are some tips for using it! :
Use the drop-down box located in the bottom left hand corner to select the category that you want to search. The 4 categories are type of space, quality, neighborhood, and amenities. To narrow down the locations shown in the map, you can select one group or multiple groups shown as the colorful circles to the right of the drop down box. For example, “Type of Space” would be the category, and “Store with Produce, Agency, and Public Space” would be considered groups. You can further target your search or search by other criteria by changing the category from the drop down box and selecting additional groups to the right of the box. As you select the groups, they appear in gray boxes, and if you want to delete a selection, just click the “X” on the left hand side of the gray box.
Here is what you will find within each category.
Type of Space:
- Stores with produce- includes grocery and convenience stores
- Agency- social service agencies
- Public Space- free space for exercise such as parks
- Gym- locations of gyms to engage in physical activity
- Healthcare- locations to access health screenings or vaccinations
- Recreational Facility- locations of community centers
- Other- locations that do not fit into the previous categories such as libraries where access to a computer is available
Quality:
- Healthy Living- includes locations for accessing healthy lifestyles
- Healthy Eating- includes locations with fresh produce or healthy food options
- Active Living- includes locations that offer free or low cost opportunities to exercise
Neighborhood: If applicable, the locations are broken into which neighborhoods the assets are located. For example: Lacy Lakeview, Kendrick, Bellmead, University, Waco and Others.
Amenities: If available, different assets are listed such as locations where playgrounds are located. For example: Playgrounds, outside fields, Library, fresh produce, school w/ playground, Playgrounds and Others.
The colorful circles on the map represent the groups within the different categories you have selected, which is shown in the image below. Click on a circle inside the map to see detailed information about the location. To look at another location click the “X” on the right hand side of the box or simply click on another circle.
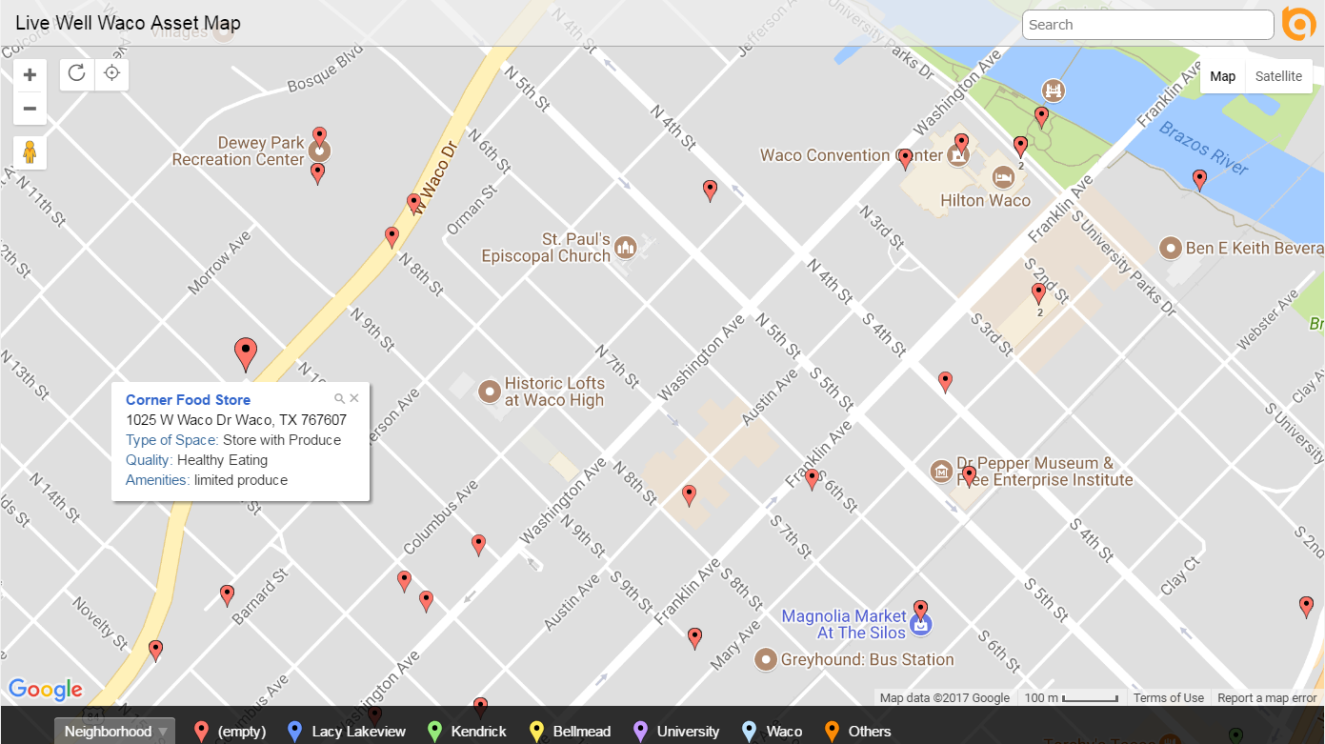
To view a list of all the locations shown on the map, first, make sure your cursor is not hovering over the map and then scroll down the page. Under the black square you will see the locations itemized in a list format. This list will change as you select specific categories and groups. You can also use the scroll bar located on the right hand side of the page.
To zoom in and out of a specific area on the map: (1) Use the + and – signs located on the left hand side of the map (2) Click on the map in the area with the circles and use your mouse to scroll forward to zoom in or backwards to zoom out.
The Live Well Waco Asset Map is an awesome tool that helps providers and community residents identify assets and strengths around the community. Types of resources are clearly and easily categorized into stores with produce, local agencies, public spaces, gyms, healthcare facilities and recreational facilities across the great City of Waco, Texas. The LWW Asset Map can save you time and money as well as improve your quality of life, so let’s SHARE it! By promoting the LWW Asset Map tool within local clinics, doctor’s offices, local food banks, and through other local organizations, we can provide this asset map as a public service to the entire community so that patients, clients, and partners can support and encourage one another to make healthier lifestyle choices. The LWW Asset Map is already linked to the Live Well Waco website, but the opportunity to spread awareness of this great resource on other organizations’ and partners’ websites will go a long way.
The Asset Map tool not only provides a visual representation of local businesses and resources, but it also provides valuable information that will ultimately help all community residents lead a healthier lifestyle. The time to improve healthy eating and increase physical activity is NOW! Let the Live Well Waco Asset Map guide you to health and success! Although the journey is not easy, Live Well Waco Coalition challenges you to take the highway and merge into a healthier lifestyle!
 CeRon Ford moved to Waco in August 2013 to attend Baylor University. He received his Bachelors of Science in Public Health, and had the opportunity to intern at the Waco-McLennan County Public Health District as a Live Well Waco intern during his final summer in Waco. CeRon will further his efforts of pursuing public health by attending Morehouse School of Medicine’s Master of Public Health Program in Atlanta, Georgia, In the Fall 2017.
CeRon Ford moved to Waco in August 2013 to attend Baylor University. He received his Bachelors of Science in Public Health, and had the opportunity to intern at the Waco-McLennan County Public Health District as a Live Well Waco intern during his final summer in Waco. CeRon will further his efforts of pursuing public health by attending Morehouse School of Medicine’s Master of Public Health Program in Atlanta, Georgia, In the Fall 2017.
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.
By Ashley Steenberger
“Doctors need to be more compassionate. First pregnancy I felt like I was just a statistic. I’m just going to rush you and get you out in 15 minutes. I’m not going to get paid that much anyways. It’s not about that. It’s about making me feel more comfortable in my pregnancy. Letting me know the risks and what can go wrong and what can go right.” — Patient Participant
 If you’ve never heard about the Healthy Babies Coalition (HBC), we are a group of dedicated community agencies in McLennan County that provides services to mothers and babies. Our focus as a coalition is to reduce existing health disparities, improve birth outcomes of mothers and babies, and improve women’s health throughout the life cycle. Currently, we meet on the third Thursday of every month from 2-4pm.
If you’ve never heard about the Healthy Babies Coalition (HBC), we are a group of dedicated community agencies in McLennan County that provides services to mothers and babies. Our focus as a coalition is to reduce existing health disparities, improve birth outcomes of mothers and babies, and improve women’s health throughout the life cycle. Currently, we meet on the third Thursday of every month from 2-4pm.
In order to better understand the barriers to accessing women’s healthcare and decreasing preterm birth and infant mortality, the Healthy Babies Coalition partnered with the Prosper Waco Women’s Health Workgroup in 2015 to conduct eight focus groups and one interview with Waco community healthcare providers, patients (women of childbearing age) and patient support systems (men and grandmother type supports). The focus groups were implemented to gain information regarding the community’s knowledge and perception of women’s health services in the community and its relation to our birth outcomes.
We received a lot of helpful data that have informed and shaped our work as a coalition and our community to better serve the women of McLennan County. Among one of the most powerful statements we heard from the focus groups was the previously mentioned quote from a female patient: “Doctors need to be more compassionate. First pregnancy I felt like I was just a statistic. I’m just going to rush you and get you out in 15 minutes. I’m not going to get paid that much anyways. It’s not about that. It’s about making me feel more comfortable in my pregnancy. Letting me know the risks and what can go wrong and what can go right”.
It is no secret that doctors are busy- they have a schedule to stick to throughout the day and that often leaves little time to address all of your concerns. But, there are ways you can play an active role in ensuring you make the most out of the time you do get with your physician as this is also your responsibility as the patient.
Here are a few tips that can help you talk to your doctor and ensure a quality appointment time:
- Write down a list of questions and concerns before your appointment. If you have a health issue, make sure to include any symptoms you may be having, when they started, how often it happens, and if it prevents you from doing something. Tell your doctor you have this list and share it with them.
- Be honest and open. Clear communication is vital in ensuring the smartest decisions are made for your health. It will help your doctor better understand your lifestyle and the best treatment choices for you.
- Consider bringing a close friend or family member with you. They can help calm your nerves as well as help you remember the tips your provider may share with you.
- Take notes about what the doctor says, or ask a friend or family member to take notes for you. If you don’t remember what the doctor shared with you, you can easily look back to your notes for reference.
- Learn how to access your medical records so you can keep track of test results, diagnoses, treatment plans, and medications and prepare for your next appointment.
- Ask questions– especially if the information you are hearing seems confusing or unclear.
- Ask for the doctor’s contact information and his/her preferred method of communication in case you have further questions or concerns.
- Remember that nurses and pharmacists are also good sources of information and can be very helpful in your health journey.
Above all, remember that you and your doctor are a team and your relationship is a partnership. You can and should work with your provider to solve your medical problems and keep yourself healthy. Your health is important so make it a priority. Take an active role in this partnership to ensure the healthiest you!
 Ashley Steenberger is a second year Master of Public Health student at Baylor University from Northwest Arkansas. Currently Ashley works with the Healthy Babies Coalition as the Healthy Texas Babies Grant Graduate Assistant at the Waco-McLennan County Public Health District and an Intern with Nurse Family Partnership Waco.
Ashley Steenberger is a second year Master of Public Health student at Baylor University from Northwest Arkansas. Currently Ashley works with the Healthy Babies Coalition as the Healthy Texas Babies Grant Graduate Assistant at the Waco-McLennan County Public Health District and an Intern with Nurse Family Partnership Waco.
By Vera Minot

(how I feel about running, most days)
When I arrived in Waco in 2013 I had no idea that my cross-country upheaval would catalyze an entire health and wellness journey for me. I began researching nutrition and preparing my meals at home, and to complement this I began working out in a gym (for a while), and I even (gasp! This part was hard) started running again. I was training for my first 5k (a big deal for me!), with bigger dreams to come, when I was hit by a car on my way home for lunch one day. As I began nursing several spinal injuries, I came to find I could no longer walk for extended periods of time without debilitating pain, let alone run. Facing potentially lifelong demobilizing injuries, I ceased my workout routines, further increasing the wellness void I had been looking to fill since arriving in Waco. I needed to find an activity that would honor my injuries, aid in my healing process, and give me the physical outlet I yearned for, I turned to that in which I had only dabbled in the past: yoga.
I started practicing yoga consistently in June of 2016, and I found that when I did my back pain decreased! Despite there being limitations to the poses (or asanas) I could perform due to my injuries, as the weeks went on I noticed I was gaining some strength in my arms, core, back, etc. Yoga seemed to be the perfect solution for what I was seeking! What I didn’t realize yet was that physical benefits are only a small part of what yoga has to offer to any one person. My journey may have begun as one of physical health, but after 7 short months I can see that while the physical benefits are many and varying, the mental health benefits greatly exceed any expectations I didn’t even know I should have.

(child’s pose, or balasana, a common resting/healing pose)
I’ve been an anxious person for as long as I can remember—I’m very self aware, so I mull over past events looking for cues for how I can better myself (“oh gosh, I didn’t ask her enough questions about herself! I need to make sure to do that more, I hope she didn’t think I was egotistical?!”), and when I’m not doing that I’m often considering the various [typically disastrous] ways a near-future event may pan out (“ok, maybe I’ll invite her for a hang out next week and I’ll make sure to ask her what she likes to cook and focus on her, but what if she thinks I’m prying? Maybe a hangout next week is too soon?”). Long story short, living in the present hasn’t always been easy for me, and unfortunately anxiety resides and thrives when I focus on the past and the future. This is where yoga comes in.
Since beginning my practice, not only have the frequency and intensity of my anxious moments decreased drastically (I realize anxiety manifests differently for everyone and as such it’s very much an umbrella term), but I’ve noticed more specific benefits to my mental health as well. Naturally, there’s the obvious increase in endorphins that happens with any exercise. There’s also the incredible sense of pride and accomplishment I feel when I make progress with an asana I wasn’t able to perform before. Perhaps most importantly though, I have increased concentration and focusing abilities (especially when it comes to doing tasks I didn’t really want to do, like vacuuming my house and going to work 🙂 ), I find that I am able to stop, breathe, think, and then act as opposed to charging forward with my conditioned, emotional reactions, and best of all my tolerance for stress and stressful situations has increased significantly!
A personal example of these benefits presented itself recently when I had to have some tough conversations with a good friend of mine. Our friendship had gone awry, and as you can imagine the conversations that can ensue around a situation like this tend to be very emotionally charged. Both of us were upset, and in that moment I would rather have been anywhere other than on her couch, talking about whether this friendship was worth continuing. In the past I probably would have written an impassioned letter, detailing every wrong, every hurt, regardless of its necessity, and then run away so I wouldn’t have to see the fallout. Present “me” was able to sit through the “awkward” silences in the conversation that night, stay true to my needs and boundaries, and respect my friend despite the incendiary nature of some of the accusations being hurled my way. We weren’t able to resolve our issues, but I was able to move forward with a sense of calm acceptance I know would have been foreign to me even 2 years ago. I credit yoga 100% for arming me with the skills to handle that situation.

(this is me doing Bakasana, or Crow’s Pose, one of the first times I was able to successfully do it! Still working on the form of course)
The benefits to my mental health since beginning my consistent practice have been so great that naturally I began to wonder why. I’m by no means a voice of authority on the scientific relationship between yoga and mental health, but here’s what I’ve found—it all seems to come down to the same couple things. BKS Iyengar, the esteemed founder of Iyengar Yoga, said “Penetration of our mind is our goal, but in the beginning to set things in motion, there is no substitute for sweat.” What we practice physiologically develops new habits and reconditions old ones that affect us mentally. When we breathe through a difficult pose, breathing deeper into the muscle or joint that’s struggling, we learn how to endure a stressful situation. When we focus on keeping our inhales and exhales even and slow to regulate our heartbeat, this keeps us in the present moment (being in the present moment is also called mindfulness)—this in turn quiets our mind, which is key in increasing concentration and focus. Mindfulness is grounding, and neurologically this helps train the brain to stay in executive thinking mode (this is where the stop, breathe, think, then act happens) as opposed to the more primal fight/flight/freeze mode. When we are practicing our balance, we are attuning to our body, making the tiny adjustments necessary to stay in a pose. Learning to attune to my body has helped me recognize the physiological precursors to stress and anxiety so that I can deal with them with a calm mind and heart as opposed to letting them overtake me.

(Kim and her daughter in the studio foyer, photo credit Sarah Hill Photography)
There are some yogis and yoginis out there who learn these lessons on their own, in their home practice. I, however, benefit greatly from a teacher’s guidance, so I’m so grateful that Yoga8 exists here in Waco. I’ve experienced all the studios in town, but when it comes down to it the feeling of love and acceptance for who I am and where I am in my journey that I feel at Yoga8 is unparalleled elsewhere, in my opinion. Kim, the owner of the studio, has a beautiful spirit as well as an incredible knowledge of the human body and its capabilities, and all of the other RYT-200 certified teachers at the studio truly take to heart Kim’s mission when she opened Yoga8 two years ago. Their mission is to improve as many lives as possible.
My short time with Yoga 8 has truly revitalized me. My time spent in their myriad classes, from the restorative Healing classes to their sweatier Kick-UR-Asana classes (and any of the classes in between) has taught me how to attune to/regulate my body and be mindful whether my toes are on the mat or not. The lessons I’ve learned and will continue to learn as I progress in my yoga journey have dramatically increased my mental health, and as such improved my life. To Kim, I can say: mission accomplished.
 Vera Minot is a reluctant adult from Arizona trying to navigate life in Waco and in this world. She finds joy in cooking, gardening, her cats, social justice, creative endeavors, books, and of course yoga.
Vera Minot is a reluctant adult from Arizona trying to navigate life in Waco and in this world. She finds joy in cooking, gardening, her cats, social justice, creative endeavors, books, and of course yoga.
By Kodie Talley
“All behaviors come from underlying desires and changing the root cause of that behavior could have more affect.” – Anne Hsu, a Behavioral Scientist at Queen Mary’s University of London.
Chocolate. Cookies. Brownies. I crave all the yummy creamy delights with ice cream on top! For a while I was eating ice cream every single night…sometimes even in replacement of dinner. I’m not kidding. I thought that since I spent an hour at the gym it wouldn’t matter. And then I wondered why I wasn’t seeing progress on my weight and health goals!
As a fitness coach and health advocate, I hear from a lot of people who get discouraged because they work so hard and yet they aren’t seeing the results they envision. It’s difficult to desire progress and use it as your motivation each day only to feel you have not improved months later.
Well, something many of these people have in common is submitting to their cravings. Even if it’s not every day it can still make an impact on your progress. Oftentimes, people will eat clean for 5 days and allow the weekends to be a free for all with alcohol and all the foods they restricted during the week (pizza, burgers, ice cream). Even if you’re eating clean most of the time, all the garbage you’re allowing two days of the week is going to set you back.
Many people try to take an 80/20 approach to their diet. This means that 80% of the time they eat clean, and 20% of the time they give in to their food cravings. But what people don’t understand is that the 20% doesn’t mean 2 days out of the week you can just eat whatever your heart desires all day long. In my opinion, what 80/20 really means is Saturday you allow yourself the bowl of ice cream (but let’s not go crazy, only have 1 serving (3/4 cup)). And then maybe Wednesday you treat yourself to a dinner out. Another example is, if you have a wedding or a dinner party, or some social event, you can eat the food! Use that as your 20%, just plan ahead.
Personally, I follow a 90/10 approach to my diet. This means 10% of the time I give in to my cravings. It’s typically about 1 weekend a month and it usually falls on some holiday or monthly celebration.
Here are a few ways to get rid of your food cravings to stay strong during your 80%:
1) Distract yourself – The theory is that cravings are caused by your imagination – imagining how good that ice cream is going to taste. According to some recent research by Anne Hsu, a Behavioural Scientist at Queen Mary’s University of London, “If you hijack that part of the brain [that is imagining the food] then it can’t sustain the craving anymore. ” In her research she used an app to get people to imagine something different – a forest, or a white horse, for example – when they felt a craving. The results showed significant reductions in unhealthy snacking. A different study recently showed that the computer game Tetris, if played for just three minutes, can weaken cravings for food.
3) Find alternatives – Try grapefruit, small red baked potatoes, carrots, and salads filled with greens and fiber. These foods work by filling people up quickly, but they all work by buying time, particularly the grapefruit as the slow, strategic method of eating one can lead to a craving forgotten. This is according to Mary Beth Sodus, a Nutritional Therapist and Registered Dietician at the University of Maryland Medical Center.
4) Be Mindful – When you try these alternatives be MINDFUL about it. I’d advise, if you’re craving ice cream, eat something that has the same texture as ice cream, maybe some healthy yogurt (you could even freeze the yogurt). While you’re eating this alternative close your eyes and feel the food on your tongue. Let your taste buds savor it.
5) Attack the root cause – Think about why you’re craving this food item. Is it because you just finished dinner and you want dessert? Maybe you’re an emotional eater and something’s bothering you. Or quite possibly you’re just bored. Be mindful of the root of your cravings and maybe you can change something about the underlying cause.
 Kodie Talley graduated from the University of Idaho with a B.S. in Exercise Science and Health and a minor in International Studies. She hopes to use her degree to pursue a career in Fitness Entrepreneurship and travel abroad to serve underprivileged communities. Kodie is originally from Washington State and moved to Waco in May 2016 to intern at the Health District and live with her significant other who is attending Baylor for his masters. So far she is loving Texas and how welcoming the Waco community has been!
Kodie Talley graduated from the University of Idaho with a B.S. in Exercise Science and Health and a minor in International Studies. She hopes to use her degree to pursue a career in Fitness Entrepreneurship and travel abroad to serve underprivileged communities. Kodie is originally from Washington State and moved to Waco in May 2016 to intern at the Health District and live with her significant other who is attending Baylor for his masters. So far she is loving Texas and how welcoming the Waco community has been!
The Act Locally Waco blog publishes posts with a connection to these aspirations for Waco. If you are interested in writing for the Act Locally Waco Blog, please email [email protected] for more information.